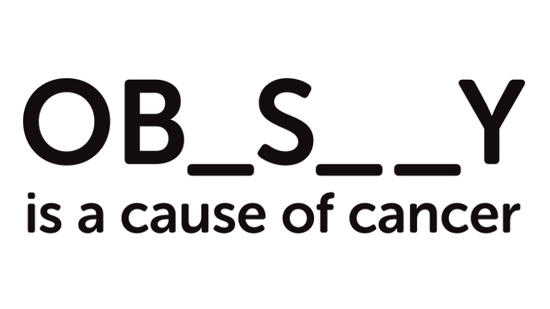
The controversial Cancer Research UK advert.
Obesity – a body mass index (BMI) >30kg/(height in m)2 – is both common and a controversial topic.
Questions about obesity
Is BMI accurate?
Well…yes. And no. So sort of both.
The body mass index is inaccurate in certain circumstances but not as wildly inaccurate as is often implied. I’ve worked mostly in deprived areas. The issue is rarely that my patients are bodybuilders or rugby players. Their increased BMI is almost invariably due to excess abdominal fat.
Like any measure in medicine – heart rate, blood pressure, Glasgow Coma Scale, blood sugar, cervical dilatation in labour – it fits as part of a wider clinical picture. No, it shouldn’t be used alone but it remains useful for assessing and stratifying patients.
If you’re Mathieu Bastareaud then perhaps BMI is irrelevant. If you’re not, you should probably take your BMI seriously.
Does being fat cause cancer?
The advert pictured is the one that made me start writing something about this, alongside comedian Sofie Hagen’s objections to it which made various news outlets. The issue? “It’s only a correlation” or “no causative link has been proven”.
Well…Cancer Research UK begs to differ. It proposes three main ways. Fat secretes oestrogen, secretes insulin and IGF (insulin-like growth factor), and causes inflammation. These 3 processes cause more cell division. Cancer is uncontrolled cell division (essentially a growth that will not stop). So the more these 3 processes occur, the more cell division there is and the more likely it is that cancer will develop.
Obesity is correlated with cancer; few dispute this. Moreover, there are pretty solid biological mechanisms by which this may occur . Whilst more research should be done, it comes down to this: nothing in medicine is perfect.
Few things that we make claims for or do in medicine have the sort of evidence that the obesity-cancer link does. Indeed, if this is insufficient, then close every intensive care unit (ICU) in the world.
About the only things we’re sure about in ICU is timing of percutaneous tracheostomy makes no difference, lung-protective ventilation is good and restrictive transfusion strategies are probably better than liberal ones. There is lower-level evidence for other stuff but, like obesity, there is so much going on in ICU, it is difficult to isolate specific causality. However, far, far more research has been done into obesity, not least because there are way, way more patients.
Can you be “fat but fit”?
Or more correctly the MHO or “metabolically healthy obese” individual. These are folks who, when they have a variety of investigations, appear “metabolically healthy”.
Whilst this study and this study both in well-respected journals in their specialties suggest MHO is not associated with increased mortality compared to the healthy non-obese, there are plenty more which dispute the definitions, its existence or whether it is any healthier. This paper suggests that MHO is mostly a transient state that will become metabolically unhealthy obesity with time.
It’s not uncommon to see articles cherry-pick a study supporting MHO. Always be skeptical. Obviously, being fit and obese is better than being unfit and obese. But being fit and non-obese remains the healthiest option.
Bottom line: obesity is very likely to be bad for your health and is a cause of cancer.
How to lose weight (in your mind)

This “obesity map” shows all the factors which lead to obesity. Source
Sure, at a personal, physical level it’s about reducing calories, reducing calories and reducing calories. And slightly about exercise. But seriously – it’s all about reducing calories. But on every other level, obesity is terribly complicated as this image shows.
However, the National Institute for Health and Care Excellence (NICE)’s guidelines have very little about what psychological advice to give to a person trying to lose weight. We know that we unfairly stigmatise the obese, that that stigma becomes internalised, and that the stigma is harmful to our patients. Moreover, the internalisation itself has correlations with poorer physical health morbidity and mental health morbidity (morbidity meaning other diseases). Thus, fat-shaming almost certainly does harm and is probably associated with poorer health.
What should doctors actually say to obese patients?
I mean, actually, literally what words should come out of the doctor’s mouth? If a patient walks into a GP’s consulting room with a lower respiratory tract infection requiring antibiotics, is this the time to bring up a patient’s weight? What about a woman with a BMI of 43.3 (5’7″, 20st) who attends for her 12-week scan? Or after 3 months coming off a ventilator because, at their weight, they really shouldn’t have been having their hip replaced (I speak from experience on this one)? And if none of these…when?
This paper by Rand and colleagues entitled “It is not the diet; it is the mental part we need help with.” looks at the myriad non-physical causes of obesity. To put this more crassly, why do obese patients keep picking up the fork?
If somebody presents with obesity, giving them advice about dietary changes is rather like telling footballers they need to score more goals than the other team or this advice from Sir Ian McKellen on acting in Extras. Whilst superficially true, it gives no insight on how to complete the task.
(As an aside, it is worth noting there are patients, particularly in poorer areas, who genuinely will not have insight into their condition. It is still worth pointing out they need to lose weight to be healthier/score goals to win.)
A 2015 systematic review by McGuigan and Wilkinson demonstrates that obesity is associated with healthcare avoidance, in part due to perceived or actual discrimination. If patients think healthcare professionals will be mean to them, they won’t seek healthcare.
Obese patients will respond poorly if they’re depressed, anxious, suffering from post-traumatic stress disorder, and/or any other mental illness or psychological issue. The causality goes both ways. Depression probably causes obesity as much as obesity causes depression. The latter will be created or at least reinforced by aforementioned societal stigmas.
Bottom line: psychology and mental health are probably as important as calorie-counting in managing obesity (and doing exercise but honestly it’s almost all about diet, exercise is good for you on its own terms).
What does it all mean?
If you deny BMI is useful, you’re wrong. But we ought to ask more about mental health, rather than simply doling out dietary advice.
Ultimately, the UK does a bad job of tackling these factors but in part, for healthcare professionals in all professions, one shouldn’t underestimate how difficult discussing obesity is to do well. I’d be intrigued to know if there is a study where the first step in discussing a patient’s obesity was to talk about their mental health.
PS: the lower respiratory tract infection was probably a virus.